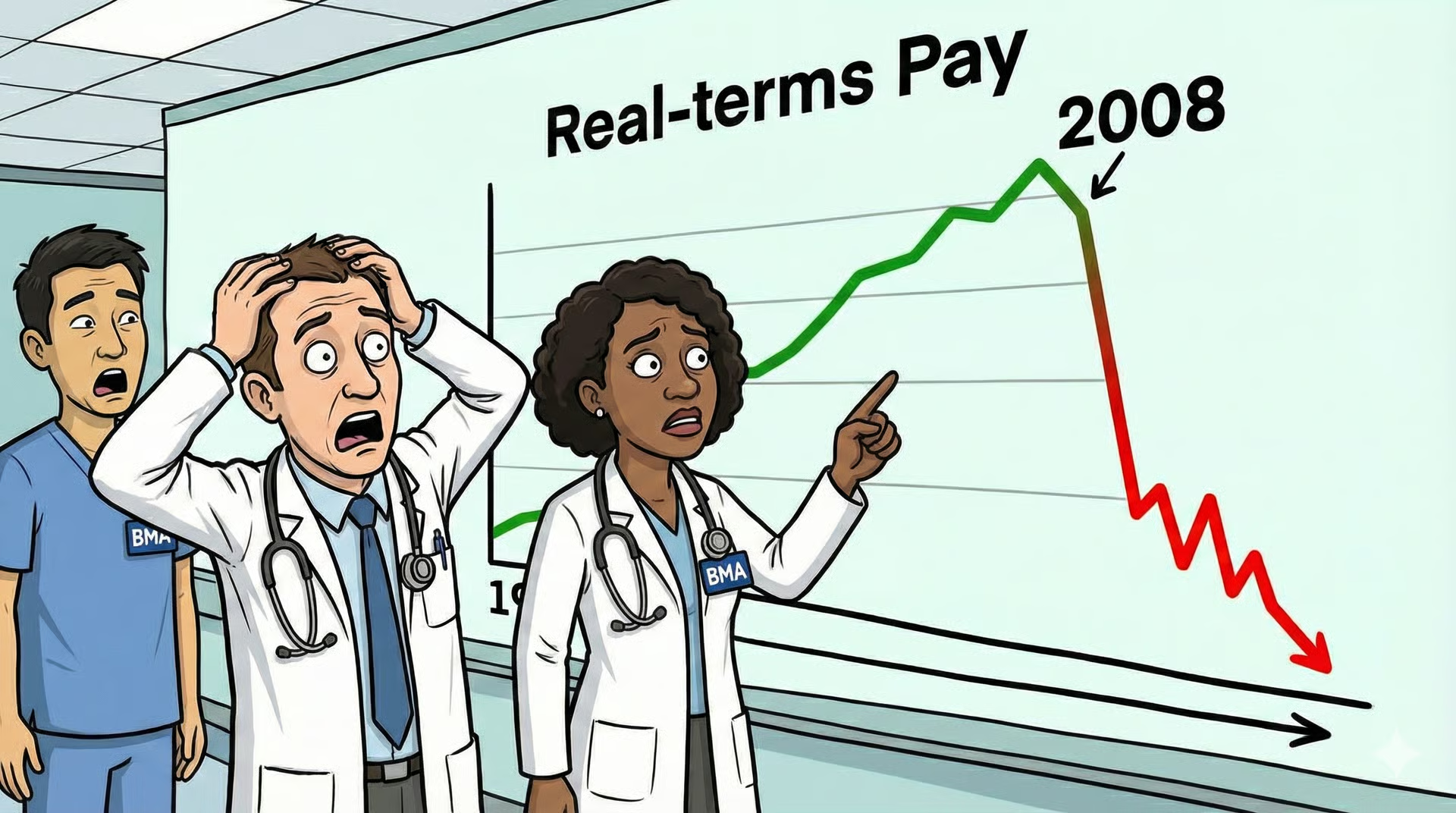
What’s So Special About 2008?
Is the BMA right to use 2008 as the benchmark for pay erosion?
What’s so special about 2008? Barack Obama became the first African American president to enter the White House, Federer and Nadal played what many consider the greatest ever Wimbledon final, Spain lifted the European Championship, and the housing bubble resulted in the global financial crisis.
The year is also relevant to us doctors for another reason. It is the year selected by the BMA as the baseline against which to compare their current real-terms pay erosion.
But is it correct to use 2008? And what would the figures look like if we use another starting point? Analysis from the Nuffield Trust shows that through the 1990s and 2000s, resident doctors received healthy real-terms pay rises, before things took a turn for the worse in 2008/09.
To show this clearly, see this beautiful graph in the same Nuffield paper. So the BMA have decided to compare members’ pay with one of the high points, in real terms, across the last 35 years. It is true that if baselines in the mid-1990s or the 2010s were used, then the headline loss would be much lower.
Importantly, none of these statistics can tell you how much doctors are ‘worth’. There is a very real argument that those persistent, above-inflation pay rises over a long period indicate that, for decades, the state repeatedly judged doctors’ labour to be valuable enough to merit those real-terms increases (even whilst restraining pay in other areas). Doctors did not become less skilled or trained after 2008.
It could be argued, in another tone, that past pay levels were contingent on economic growth, political choices, fiscal capacity, and the relative scarcity of skilled labour. The pay rises leading up to 2008 were not moral guarantees, but the outcome of specific UK circumstances. As competing priorities emerge, such as the booming social care budget, a change in the geopolitical landscape that made leaders think about increasing defence spending, and demographic shifts, the social contract needs to be renegotiated.
The strongest objection to using 2008 as a benchmark is not statistical but philosophical. Historical pay levels, however sustained, do not automatically generate moral entitlement. They are the product of contingent economic conditions and political choices, not guarantees written into a social contract. A society is entitled to reassess how it values and remunerates professions as circumstances change. From this perspective, invoking a bygone high point risks mistaking historical advantage for an established right.
So when we ask ‘What year is correct?’ we might be asking the wrong question. It may very well be easier to arbitrarily pick a year and campaign based on a number, because pay is a convenient benchmark. But a number cannot capture the cumulative effects of policy decisions and societal expectations, nor does it reflect the changing demands of society.
Weekly Prescription
The Academics Pushing a Minimum NHS Service Period For UK Doctors
The ‘minimum NHS service’ argument appeared in the Journal of Medical Ethics earlier this month. For those unfamiliar, the policy calls for a minimum period of NHS service for UK-trained doctors, akin to our military doctor colleagues, who serve a minimum number of years in their respective forces upon graduation.
The reason for the recent attention is that the most recent 2024 estimate suggests that the investment cost to train a doctor through to the point at which they receive full GMC registration amounts to £374,895. This cost is shared between the taxpayer and the individual undertaking their training, with the net cost to the taxpayer estimated at £250,000.
The author argues that the policy would operate such that if UK-trained doctors wish to no longer practise medicine in the NHS during this period, they would have exit options. These would include either paying the associated costs (through a lump sum, monthly payments, or tax code adjustments) or working in alternative roles within the NHS until the service requirement has been satisfied.
The authors do recognise, however, that such a minimum service obligation would struggle to function without satisfactory working conditions first and appropriate remuneration for doctors working in the NHS. Our military colleagues are financially remunerated for their service, as well as receiving a range of other work-related benefits. So what do you think? Does this policy have any real prospects in the future of the NHS?
What is The BMA’s Grandfathering Policy?
Why UK graduate prioritisation is not as straightforward as it might seem
The policy of UK graduate prioritisation continues to make headlines following the recent proposal by Streeting to avert strike action. We know that the idea of prioritising UK graduates is something the government is taking seriously, but many in the public and within the NHS want clarity on the details, such as whether this policy would apply solely to speciality training posts or whether it would also extend to trust grade posts.
One of the most consequential questions concerns International Medical Graduates who are already working within the UK. For this group, the current period is likely to be one of considerable uncertainty as they await further direction from the government. This uncertainty is not trivial. Over the past five years, the proportion of BMA membership composed of IMGs has grown substantially, to the point where they now constitute a sizeable minority within the union and the workforce more broadly. Any policy shift in this area, therefore, carries significant implications for industrial relations, workforce stability, and morale.
Current BMA policy for IMGs who are already GMC-registered and working in the UK is known as grandfathering. In practical terms, this refers to a commitment that IMGs already contributing to the NHS would not find themselves abruptly excluded from training pathways. Under this policy, the BMA states that any IMG who has completed two years of NHS experience as a medical doctor should be granted equal access to speciality training alongside UK graduates.
If this approach is maintained, it is unlikely that UK graduate prioritisation will materially ease the competition ratios currently seen in speciality training. By the time any such policy comes into force, most doctors already in the system will fall within the scope of grandfathering protections. As a result, the immediate pressure points driving discontent among UK graduates may remain largely unchanged. This helps explain why enthusiasm for the policy is far from universal among doctors, despite its intuitive political appeal.
Board Round
A round-up of what’s on doctors’ minds
“There are some statistics that NHS leaders and government officials obsess about, and one of them is the elective backlog and waiting time. I am sure they are acutely aware that the only way to tackle these numbers is a greater expansion of the Consultant and GP workforce.”
“Do you think Jack Fletcher and the BMA should be utilising more real (absolute) terms language, i.e. £18/hr instead of relative term language (28% rise)?”
“It should be a matter of pride and good manners for the surgical team to manage a post-op infection that presents to the ED.”
“The first systematic review you ever attempt is going to break you. Luckily, things smooth out after that.”
Referrals
Some things to review when you’re off the ward…
We think this is one of the best pieces of analysis from Full Fact on the erosion of doctors’ pay since 2008. It digs into figures using different inflation measures such as RPI, CPI and CPIH and shows how the choice can lead to significantly different outcomes.
Here’s a nice little new-year present for you all from the GMC. From 1st April 2026, the fees are increasing from £463 to £481, with the discounted fee (for newly qualified doctors up to 5 years post-qualification) going from £177 to £184.
Weekly Poll
In this financial year, are you expecting your student loan balance to go down?
…and whilst you’re here, can we please take a quick history from you?
STAT Note
Costing a Doctor: The UK’s £375,000 Asset
For the government, the cost of training up a doctor should be seen less as an expense and more as an asset. The total price tag to train a doctor to full registration at the end of F1 reaches £374,895, with this figure spread between the taxpayer and the individual undergoing the training. The individual doctor shoulders £114,827 of this bill, with the taxpayer investing £260,068.
This figure may surprise you or sound about right, but rather than making one scoff, it should evoke a sense of pride in our profession, as it is one that requires time and resources to achieve mastery.
How does this £374,895 number break down? Let’s have a look:
To the dismay of all those students who snuck away from placement this morning at 11 am after the morning ward round, the lion’s share of the total is taken up by clinical placements and totals £180,277. Tuition fees average £51,014. Salaries and postgraduate support total £60,055.
Interestingly, the figures group living expenses with ‘opportunity cost’, which totals £73,063. Living expenses are fairly intuitive. It is the basic cost of survival whilst in medical school, including rent, food and Wetherspoons. Opportunity cost, however, is an interesting economic concept to consider as well.
Effectively, there is some lost production when a talented student goes to medical school. If they had not done so, they would likely have been working in a high-level graduate job immediately after completing a three-year BSc or apprenticeship scheme. This figure represents the income they sacrificed to be a student. It is the cost of having a brilliant mind out of the workforce for half a decade.
Share the News. Build the Community.
Help us build a community for doctors like you. Subscribe & Share On-Call News with a friend or colleague!
*We’ve done our best to keep this information accurate, but person specifications can change. Always check the latest person specification for your training programme before relying on this information.
Disclaimer:
Content in the On Call Newsletter reflects the personal views of individual authors and does not represent the views, policies or guidance of Medset Ltd. Articles are for general information only and do not constitute clinical or professional advice. Medset Ltd accepts no liability for decisions made based on this content.